Credentials at a glance
Lisa Hardy, APRN, PMHNP-BC, CNM
Board Certification
Psychiatric Mental Health Nurse Practitioner
Certified Nurse-Midwife
Education
Yale University School of Nursing
Frontier School of Nursing
University of Michigan
Duquesne University
Clinical Focus
Women’s mental health
Hormonal & reproductive transitions
Anxiety, depression, OCD
Midlife psychiatry
Professional Memberships
American Psychiatric Nurses Association
American Association of Nurse Practitioners
American Academy of Nurse-Midwives
What is Psychiatry?
Vermonters come to a psychiatry provider looking for relief—but just as often, they’re looking for understanding.
As a PMHNP in Vermont, I specialize not only in Psychiatric Care & Women’s Mental Health in Vermont, but also in listening and understanding your story.
I’m a double board-certified Psychiatric Mental Health Nurse Practitioner and Certified Nurse-Midwife, with a clinical focus on women’s mental health, hormonal transitions, and periods of significant life change. I work with people who want thoughtful guidance, careful judgment, and care that makes sense in the context of their lives—not just their symptoms.
Psychiatric NP: Being With vs Doing To
Early in my career, I was eager to do: to diagnose, intervene, and fix. One of my first clinical lessons, however, had very little to do with action.
As a new nursing assistant on a cardiac unit, I was assigned to sit with a man who was frightened and struggling to breathe. There was no procedure to perform, no decision to make—just time, presence, and attention. Over the course of the hour, his breathing eased. His anxiety softened. Before I left, he squeezed my hand and thanked me.
What stayed with me wasn’t the medicine that helped him—it was the realization that being with someone can be as important as doing something to them.
That understanding has guided my work ever since and eventually led me to becoming a Psychiatric Nurse Practitioner in Vermont after having worked as an RN in Chittenden, Franklin, Lamoille and Washington counties as well as connecting with Vermonters all over the state.
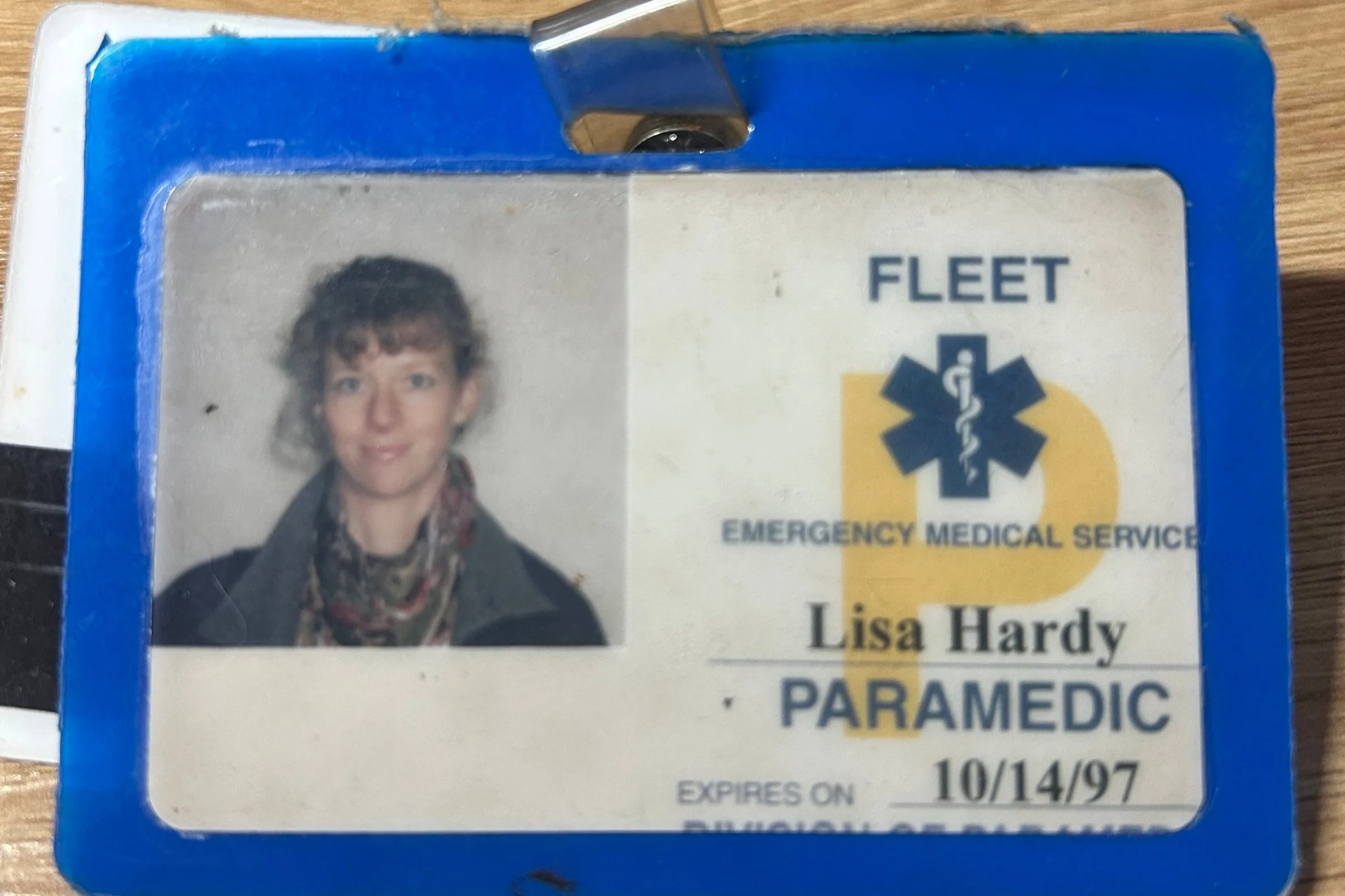
Across roles as a paramedic, cardiac technician, nurse, nurse-midwife, and now psychiatric nurse practitioner, I’ve seen this truth repeat itself: people feel better not only when symptoms are addressed, but when they are understood, grounded, and met with steadiness during uncertainty.
Psychiatric Care & Women’s Mental Health in Vermont
I created Optimind Mental Health & Wellness as a psychiatric practice in Vermont where psychiatric care is both structured and attuned. My focus is women’s mental health, but I am open to all.
I use science, data, and clinical guidelines where they are helpful in the treatment of mental disorders—and I rely on experience, pattern recognition, and careful listening when the picture is more complex than a checklist can capture.
Psychiatric medication is one tool among many. Sometimes it plays an important role. Sometimes it doesn’t. My job is not to maximize treatment, but to help determine what is appropriate, sufficient, and supportive over time.
In addition to psychiatric evaluation and medication management, my psychiatric care may include attention to hormones, sleep, nutrition, stress, trauma history, life stage, and meaning—because mental health does not exist in isolation from the rest of a person’s life.
Healing, in my experience, is not just clinical. It’s relational. And it happens best in partnership.
A little more about me
Beyond my clinical roles, I’m also a teacher, writer, and adoptive parent. I value creativity, reflection, and the ways people make meaning in their lives. These perspectives inform how I listen and how I practice. I have had a passion for women’s health for the past 35 years.
I believe good psychiatric care creates enough stability for people to reconnect with themselves—and decide what matters next.
“Nature alone cures…what nursing has to do…is put the patient in the best condition for nature to act upon them.”
— Florence Nightingale
This principle continues to guide my work.